The Nigeria Centre for Disease Control and Prevention (NCDC) has confirmed that there are four positive cases of monkeypox in Maiduguri, the capital of Borno State.
RNI reporter Ummi Fatima Baba Kyari spoke to Dr Muhammed Hashim, who works for the new GRA clinic, a primary healthcare facility.
He said the illness was a viral zoonotic infection, meaning that it could spread from animals to humans, as well as from person to person and that it was highly infectious.
People who consumed monkey meat, particularly if it was undercooked, or who came into contact with the blood of an infected animal could easily spread the virus.
He emphasised the need for people to take precautions and urged them to stop eating bush meat.
Because it was so contagious, he said it was important for people to wash their hands with soap and water regularly, particularly before and after eating.
Hashim said all eating and cooking utensils should be properly washed.
If someone was infected, he or she should be isolated and given proper medical attention. Medical personnel or relatives should wear gloves if they came into contact with the person.
He said the four infected people were internally displaced persons.
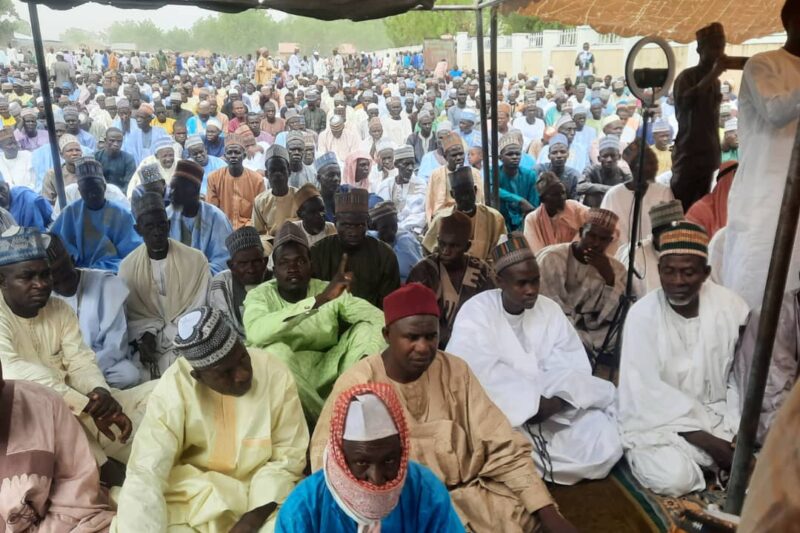
Maiduguri residents interviewed by RNI had not heard of monkeypox. They said the government should hold awareness programmes to inform and educate the public about the virus.
The World Health Organisation (WHO) said that those at higher risk for severe disease or complications included women who were pregnant, children and people who were immunocompromised.
“The most common symptoms include fever, headache, muscle aches, back pain, low energy and swollen lymph nodes. This is followed or accompanied by the development of a rash which can last for two to three weeks. The rash can be found on the face, palms of the hands, soles of the feet, eyes, mouth, throat, groin and genital and/or anal regions of the body. The number of lesions can range from one to several thousand. Lesions begin flat, then fill with liquid before they crust over, dry up and fall off, with a fresh layer of skin forming underneath,” the WHO said.
It said in some people, an infection could lead to medical complications and even death. Newborn babies, children and people with underlying immune deficiencies might be at risk of more serious symptoms and death from monkeypox.
Complications included secondary skin infections, pneumonia, confusion and eye problems. In the past, between 1% to 10% of people with monkeypox had died.
Monkeypox could be spread from person to person through close contact with someone who had a monkeypox rash, including through face-to-face, skin-to-skin, mouth-to-mouth or mouth-to-skin contact, including sexual contact. It was thought that people were infectious until all of their lesions had crusted over, the scabs had fallen off and a new layer of skin had formed underneath.
The WHO said environments could become contaminated with the monkeypox virus, for example when an infectious person touched clothing, bedding, towels, objects, electronics and surfaces. Someone else who touched these items could then become infected. It was also possible to become infected from breathing in skin flakes or virus from clothing, bedding or towels.
Ulcers, lesions or sores in the mouth could be infectious, meaning the virus could spread through direct contact with the mouth and respiratory droplets.
The virus could spread from someone who was pregnant to the foetus, after birth through skin-to-skin contact, or from a parent with monkeypox to an infant or child during close contact.
The organisation said monkeypox could spread to people when they came into physical contact with an infected animal. Animal hosts included rodents and primates. The risk of catching monkeypox from animals could be reduced by avoiding unprotected contact with wild animals, especially those that were sick or dead (including their meat and blood). In endemic countries where animals carried monkeypox, any foods containing animal meat or parts should be cooked thoroughly before eating.
People who lived with or had close contact – including sexual contact – with someone who had monkeypox, or who had regular contact with animals which could be infected, were most at risk.
The WHO warned health workers to follow infection prevention and control measures to protect themselves while caring for monkeypox patients.
UMMI FATIMA BABA KYARI